COVID-19 Clinician Surveys
3-Minute Survey Overview


The Primary Care Collaborative and Larry A.Green Center continue to survey primary care providers weekly through the COVID-19 crisis, putting a critical spotlight on primary care needs for national leaders and lawmakers. Responses to these surveys have appeared in more than 50 news stories and research articles advocating for support of primary care. In Rhode Island, CTC-RI has been able to use results to aggregate RI data to inform state health policy.
New survey links will be posted each week at www.green-center.org. All can share all data and reports for dissemination purposes both internally and externally without additional permissions, provided they attribute the data to the Larry A. Green Center.
-
RI providers are unable to hire staff for open positions (79% vs 54% Nationally)
-
RI providers have seen a rise in mental health issues among children (e.g., depression, anxiety, ADHD) (79% vs 65% Nationally)
-
RI providers are constantly worried about the poor mental health of practice members (67% vs 53% Nationally)
-
COVID-19 is again surging in my area and I don’t know if I can take it. (59% vs 50%)
-
RI providers personally know primary care clinicians who have retired early or left practice because of the pandemic (59% vs 45%) and primary care practices that have closed during the pandemic (56% vs 29%)
-
Only 18% of RI providers feel their practice is financially healthy (vs 26% nationally)
- RI providers are experiencing the following with vaccine hesitancy:
- Conversations with vaccine hesitant patients take several minutes (85% vs 80% Nationally)
- For most vaccine hesitant patients, it’s a gut or political opinion that cannot be changed (68% vs 67% Nationally)
- 2-3 conversations are needed to change the mind of vaccine hesitant people (56% vs 52% Nationally)
- For most vaccine hesitant patients, education on the issues can make a difference (44% vs 26% Nationally)
-
Use of telehealth has been essential to maintaining access to patients says 71% of RI providers (compared to 64% Nationally); however if Pre-COVID telehealth regulations are restored, practices will not be able to provide telehealth services (47% vs 41%)
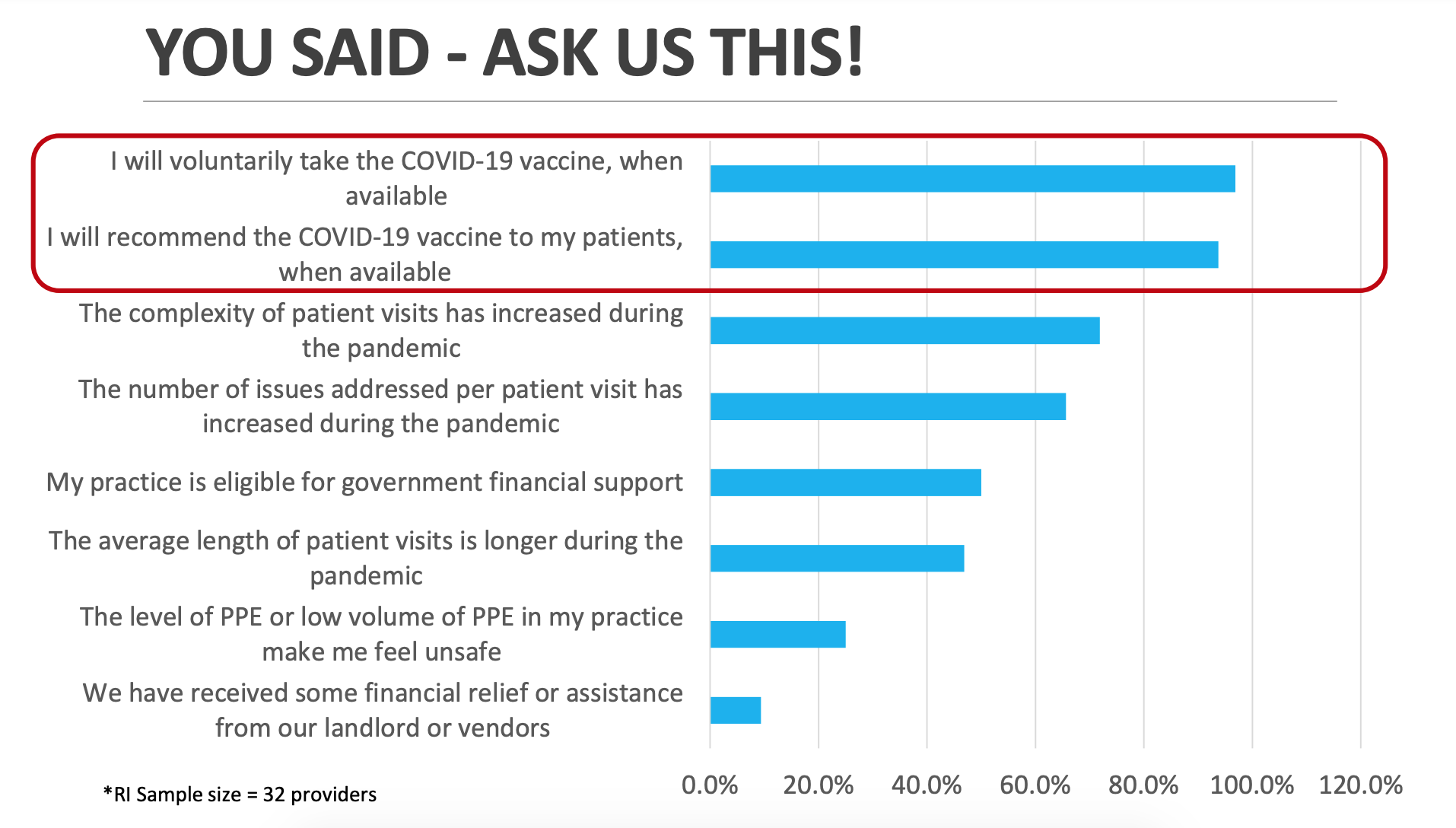
COVID-19 vaccines are now available, yet primary care remains a largely untapped resource in vaccine administration. 99% of clinician respondents believe primary care should be helping with vaccine distribution, yet only 1 in 5 are currently involved. 6 in 10 practices are willing and ready to assist with vaccine distribution but face obstacles, such as lack of storage, staffing, or PPE required. This despite the fact that primary care can help reach vulnerable and at-risk patients and has vast vaccine experience. Among respondents, 20% were practicing in rural communities, and 17% were caring for almost exclusively Medicaid covered patients, and 6 in 10 had patient panels in which at least 75% patients have multiple chronic conditions.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Primary care, the foundation of our fragile health system, is on the verge of collapse. Even as a COVID-19 vaccine becomes available, primary care faces serious threats to its capacity to triage and treat. Over half (60%) of surveyed clinicians report their patients’ health, unrelated to COVID-19, has worsened. Practices are suffering – 91% have some form of personnel shortage, 61% have severe/near severe practice stress, and 41% have staff positions they cannot fill. Primary care is critical to vaccine distribution, yet only 5% have a full plan for distribution.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
RHODE ISLAND SPECIFIC DATA
Click here for the most recent Rhode Island results by CTC-RI
As we begin month 9 of the pandemic, primary care is weaker, patients are sicker, and the pandemic is raging more fiercely. For months, medical groups have raised alarms about the escalating consequences on patients of failing to adequately support primary care during the pandemic: excess mortality, preventable worsening of non-COVID related health conditions, high levels of mental anguish, growing social needs, and surging pandemic misinformation. The impact of inaction is clear. More than half of clinicians report severe/near severe levels of practice stress and growing patient health burden due to delayed or inaccessible care. Nine months in, COVID-19 is again surging, 63% of practices have staff out due to illness or quarantine, 1 in 5 lack sufficient testing supplies, and over half report increased patient distrust of medical information from public leaders.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
RHODE ISLAND SPECIFIC DATA
Click here for the most recent Rhode Island results by CTC-RI
Seven months into the pandemic, patients are exhibiting the effects of delayed or inaccessible care. Over half (56%) of primary care clinicians have seen an increase in negative impact on patients’ health. With COVID-19 now surging beyond Spring 2020 levels, practices continue to face unresolved pressure points from the first wave, such as inability to fill open staff positions (35%), persistent challenges with COVID-19 testing (61%), and difficulty with PPE (37%). Despite this, practices are showing remarkable adaptiveness by significantly increasing their outreach to community organizations and adopting wise and flexible use of telehealth despite payment concerns.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
RHODE ISLAND SPECIFIC DATA
Click here for the most recent Rhode Island results by CTC-RI
Population health is in decline, primary care is under water, and major disruptions to medical supply chains all signal that our health system is buckling. The health of the population has weakened during the pandemic with half of clinicians noting that overall physical health of the population has declined. In addition, 41% say the health of those with chronic conditions is noticeably worse, and 86% report a pandemic-specific decline in the population’s mental health. At the same time, only 1 in 5 surveyed clinicians report their fee-for-service volume is within 10% of pre-pandemic levels and nearly half (47%) endorsed the statement that despite a somewhat rosier economic picture, their clinical workforce is fragile. Heading into flu season, shortages of PPE (33%) and flu vaccine (13%) are now a major concern.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Has primary care bounced back since the start of the pandemic? Some modest gains have happened recently but primary care remains in significant need of support: 35% say revenue and pay are still significantly lower than prepandemic levels and net losses threaten current and future viability. Another third of clinicians say the financial picture has been slowing improving but the workforce is fragile and in trouble. And 1 in 5 practices report they have clinicians who have chosen early retirement or left their jobs as a direct result of the pandemic.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
The primary care platform is shrinking. The low level and time limited support offered through previous federal relief efforts are ill-matched with the magnitude of COVID-19 challenges. In just the past month, 2% of practices have closed, another 2% are considering bankruptcy, and 10% are unable to be certain of their solvency 4 weeks out. Faced with rising population health burden, insufficient support from leaders and policy makers, and the relentless financial challenges and mental exhaustion, 1 in 5 clinicians are now considering leaving primary care and 13% could not answer that question either way.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
During month 5 of the pandemic, a tsunami continues to build within primary care while minimal public or private support is offered. The primary care platform is shrinking, the majority of those remaining work longer hours for less pay, and patient health burdens are increasing. 63% of practices note stress increasing over the past 4 weeks and report COVID-19 and non-COVID-19 illnesses are on the rise. Patient visits consistently involve greater complexity and a growing level of health burden, while more than half of primary care clinicians report their practices are short of staff due to illness/self-quarantine (53%) and additional layoffs/furloughs (22%) over the last month. Meanwhile 1 in 3 spend up to 8 hours a week trying to find COVID-19 related supplies (PPE, and swabs and reagents for testing).
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Four plus months into the pandemic, lack of substantial policy response by public or private sector leaders and a persistent dire “new normal” pose a credible threat to potential collapse of US primary care and of independent practice. Four in 5 surveyed clinicians report practice strain is worse than in March, the first month of the pandemic, with 50% saying that they are just getting used to the poor conditions. Although telehealth has proven a useful care tool during the pandemic, lack of sufficient support has resulted in a downturn in use and a choke point for patient access.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Four months into the COVID-19 pandemic, fewer than 10% of US primary care practices have been able to stabilize operations. While 13% are adapting to a “new normal”, nearly 9 in 10 practices continue to report significant difficulties whether through obtaining medical supplies, rising health needs among patients, or limited resource support. Fewer than 4 in 10 clinicians feel confident and safe with their access to PPE and 11% report practice members quit in the last four weeks over safety concerns.
NATIONAL DATA
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
This week, the survey focuses on the summer surge of cases and the preparedness of the primary care workforce for a second wave.
Thirty states across the US have experienced a summer surge of COVID-19 cases, yet more than a third of clinicians (35%) report they are not ready to address this increased patient need, despite some efforts to shore up primary care. Over 40% said they are unprepared for a second pandemic wave experts expect this Fall. Weakened finances have left primary care practices unstable at the same time that more than half of clinicians report an increase in non-COVID morbidity and mortality that appears to result from COVID-19 related obstacles to accessing health care. Mental stress on this workforce is at historic highs.
RHODE ISLAND SPECIFIC DATA
Click here for the most recent Rhode Island results by CTC-RI
NATIONAL DATA
Click here for C19 Series 18 National Executive Summary
Click here for a downloadable pdf by the Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Click here for a PDF of the Patient Series 3 Findings (fielded June 8)
This week, the survey focuses on the collatoral damage to the primary care workforce, with statements about burnout from doctors across the country.
In public and private payer responses to the COVID-19 pandemic, primary care clinicians and staff are becoming overlooked collateral damage and feel as though they have been forgotten or ignored. More than 80% are experiencing high levels of burnout and 1 in 5 have no access to known resources for support. The supply of personal protective equipment (PPE) is elusive or non-existent for many primary care practices. Clinicians and staff are worried about their healthy patients not receiving necessary preventive services; concerned their sicker patients are getting worse through care deferred or delayed; worried about their livelihoods (jobs and income), contracting COVID-19, and potentially bringing it home to their families.
RHODE ISLAND SPECIFIC DATA
Click here to download a PDF with RI results compiled by CTC-RI
NATIONAL DATA
Click here for a downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Click here for a PDF of the Patient Series 3 Findings (fielded June 8)
This week, the survey includes an important question specifically related to how George Floyd's death and the aftermath may be impacting patients and practices.
The impact of George Floyd’s death, and related protests, are compounding the stress levels in primary care practice, adding to COVID-19 related health and financial distress. This week’s survey shows that more than half of patient, clinician, and practice conversations included discussion of racism-related events and their impact on health and wellbeing, demonstrating the role of primary care practices as a relational space for everyday life and sense-making. Practices also report a disconnect that gets at the heart of primary care: more than 80% of them prioritize being the first contact for their patients with the health care system and being able to provide integrated and comprehensive care, yet only 20-37% report that they are consistently able to deliver this kind of care during the pandemic.
RHODE ISLAND SPECIFIC DATA
Click here for a PDF of the impact of COVID-19 in Rhode Island
NATIONAL DATA
Click here for a downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Click here for a PDF of the Patient Series 3 Findings
Please help share this week's Primary Care Collaborative survey to help protect and advance the needs of primary care – this is a critical time to advocate for our industry!
The vast majority of primary care clinicians (>70%) report patients as their allies and valuing their care. In stark contrast, they identify strong lack of value for primary care among the Federal government (39%), private insurers (34%), hospitals(34%), health systems (31%), and government insurers (30%). Although payment systems continue to undervalue digital health options, clinicians’ rapid adoption and use of digital health has started to reveal clear preferences. When infrastructure permits, many rate video visits over telephone calls and find virtual care is best suited for primary care based mental and behavioral health counseling and adult visits for patients with stable chronic conditions. Digital health appears least suited for assessments of injuries, non-stable chronic care, and well child visits.
RHODE ISLAND SPECIFIC DATA
Click here to review Rhode Island specific results compiled by CTC-RI using PCC survey data
NATIONAL DATA
Click here for a downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Click here for a PDF of the Patient Series 2 Findings
This week's survey focuses on questions of financial loss and sustainability. Responses were shared with senior CMS and HHS staff and leaders.
Despite 38% of practices receiving some Federal financial support, the financial pressures remain acute. Close to half of respondents have had to layoff/furlough an average 30% of their staff and 28% deferred or skipped salary payments to clinicians. For those that reported more detailed financial information, 77% reported a negative net (revenue-expenses) in April 2020 as compared to 18% negative net in January 2020. Clinicians are clear that if they are adequately supported, they will provide the kind of comprehensive, coordinated, and relationship-centered care that patients are seeking from primary care.
RHODE ISLAND SPECIFIC DATA
Click here to review Rhode Island specific results compiled by CTC-RI using PCC survey data
NATIONAL DATA
Click here for a one page downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Click here for a a one page downloadable PDF of the Patient Series 1 Findings
This week's survey has a focus on routine care delivery that is now being deferred.
After 2.5 months, primary care practices are beginning to report some modest improvements in key areas, such as an increase in testing capacity beyond CDC guidelines (29% to 35%) and reduction in percent of practices temporarily closed (19% to 12%). However, the overall picture for primary care remains tenuous with 40% continuing to report laid off or furloughed staff and 42% reporting staff out due to illness or quarantine.
Click here for a one page downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
Results from this week's survey will be sent directly to Speaker Pelosi, Minority Leader McCarthy, Majority Leader McConnell, and Minority Leader Schumer. Responses will also reach insurance leaders.
Nine weeks in to the COVID-19 pandemic, a heroic but potentially tragic story is emerging. In less than two months, clinicians have transformed primary care, the largest health care platform in the nation, with 85% now making significant use of virtual health through video-based and telephone-based care. But the large differences in terms of payment across payers is exacting a financial toll. Over 50% of clinicians report no payments received in the last 4 weeks for virtual health care, 18% report billing denied, and among those paid, over 60% report that their telehealth visits are not at parity with face to face encounters.
Click here for a one page downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
This week's survey focuses on collateral damage related to the pandemic.
After 8 weeks, primary care clinicians continue to face considerable headwinds (@ 40% laid off staff) and the future looks grim. Clinicians predict primary care will be overwhelmed with pent up demand and 38% expect to see non-COVID related deaths due to lack of access or care delayed. 66% expect increased population health burden resulting from care avoided or diverted, particularly for mental health services (74%), preventive care (72%), and chronic care (71%) visits.
Click here for a one page downloadable PDF by The Larry A. Green Center
Click here for a quick summary of the data by the Primary Care Collaborative
This week's responses were heard by over 130 Capitol Hill staffers connected to the Primary Care Caucus and Health Policy Committee.
The dire financial picture continues – 47% of primary care clinicians report they have laid off/furloughed staff, 2/3rds report that less than half of what they do is reimbursable, and 45% are unsure if they have enough cash to stay open for the next 4 weeks. With 61% of practices conducting limited or no in-person visits, it is perhaps not surprising that the 50% of clinicians are unsure about opening up the country. 39% report no connection to local health departments and 37% suggest that opening the country depends upon testing, PPE, geographic specific conditions and other factors.
Click here for a one page downloadable PDF by The Larry A. Green Center
Click here for Rhode Island-specific data
Our Mission
The mission of the Care Transformation Collaborative of Rhode Island is to lead the transformation of primary care in Rhode Island in the context of an integrated health care system; and to improve the quality of care, the patient experience of care, the affordability of care, and the health of the populations we serve.
